Whether you’re living with POTS or EDS or still searching for a diagnosis, you’ve probably found that the journey towards treatment is not easy. Patients with either condition will agree that the complexity of these disorders makes them incredibly hard for both doctors and patients to track down.
Despite the massive daily impacts of living with EDS and POTS, patient resources remain limited because of the small number of diagnoses and lack of awareness. However, with growing patient communities and growing access to information, there’s hope for bridging the resource gap and improving the outcomes for patients with POTS and EDS.
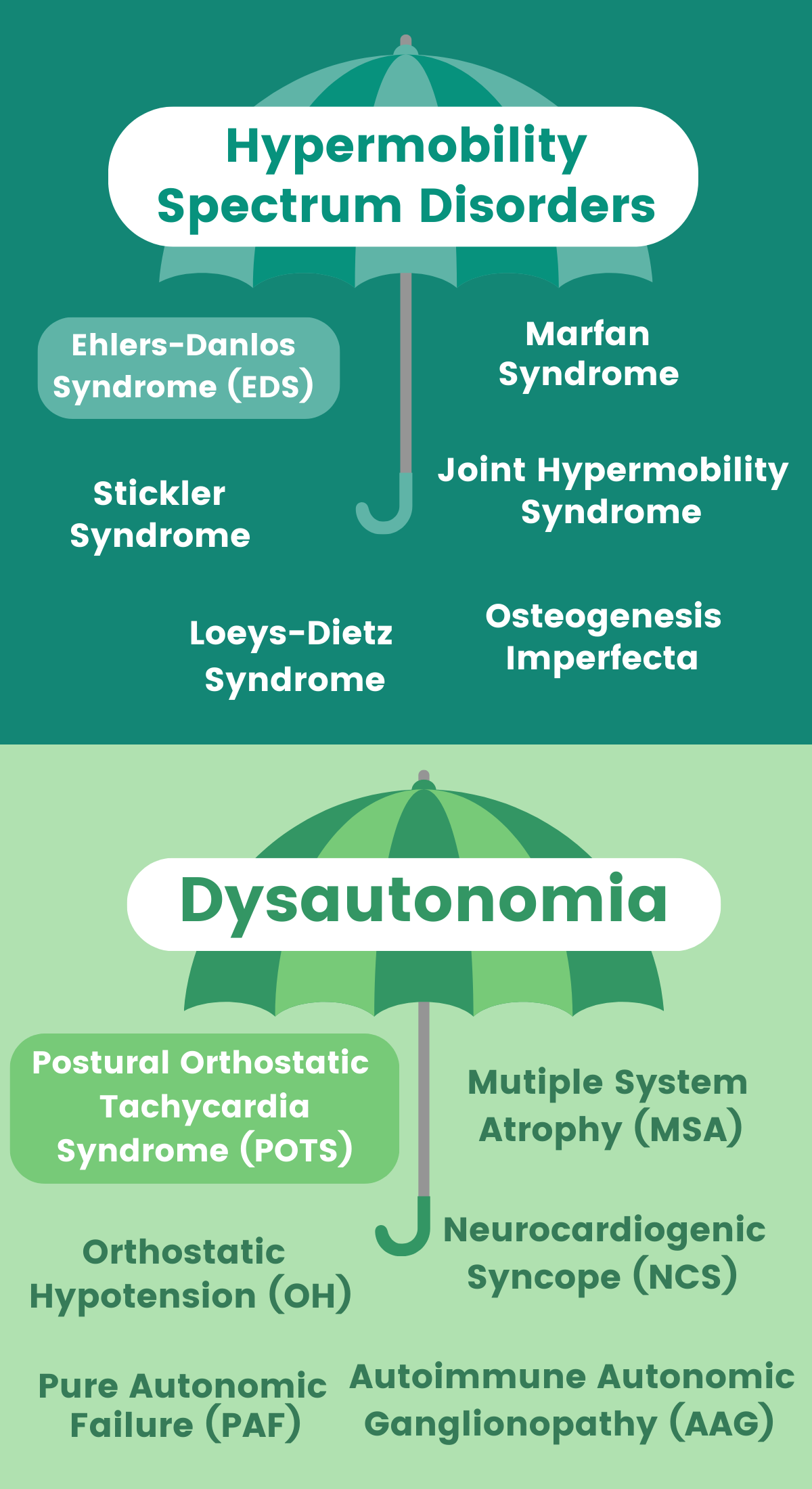
At Guava, we’re on a mission to improve access to resources for people with chronic illnesses. We're currently focused on the two umbrellas of diagnoses for hypermobility disorders and dysautonomia, the most common of which are POTS and EDS. We're chatting with users and collaborators affected by these conditions to find the best ways to improve their health management.
What is Postural Orthostatic Tachycardia Syndrome (POTS)?
POTS stands for Postural Orthostatic Tachycardia Syndrome. Unless you’re a doctor or you’re already well-versed in the condition, those words don’t exactly roll off the tongue.
When you break down the jargon, you’ll see that POTS refers to a disorder where when you stand up or sit upright, your heart starts beating abnormally fast. There are also other symptoms, like abnormally high levels of fatigue or lightheadedness, or nausea, to name a few.
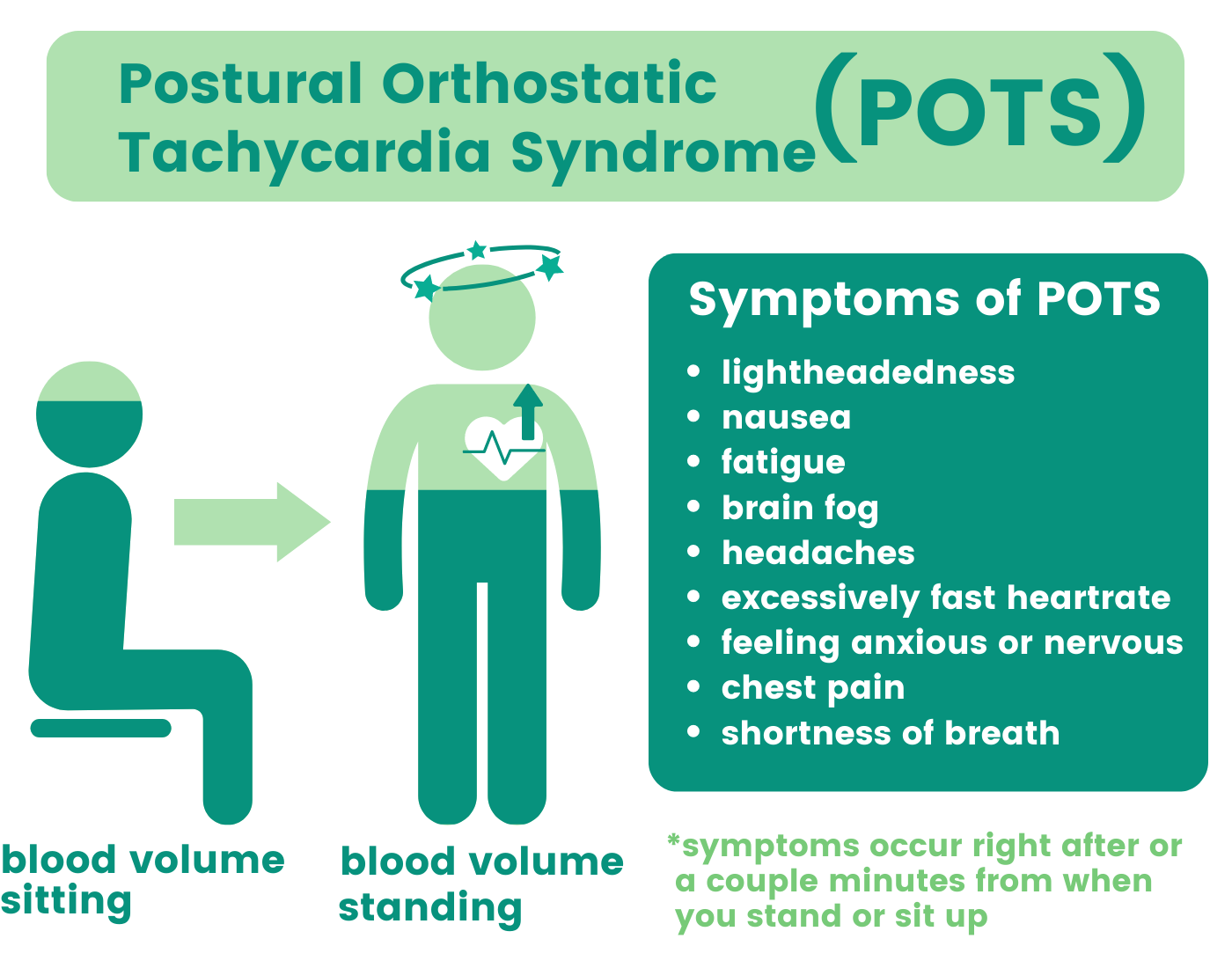
When you’re sitting or lying down, your blood is evenly distributed throughout your body. When you stand up, gravity pulls down on your blood, and your body needs to adjust to keep blood flowing steadily through your heart and brain. Normally, your body releases a couple of hormones involved in your "fight-or-flight" response, which is controlled by the sympathetic nervous system. The sympathetic nervous system increases your heart rate and constricts your blood vessels by releasing the hormone adrenaline. Adrenaline causes blood to flow back up to your heart and brain so you can react quickly to life threatening situations, hence the term “fight-or-flight.”
For people with POTS, the body’s mechanism for adjusting blood flow and heart rate in response to standing up doesn’t work properly. This is why POTS is a complicated disorder and difficult to get a diagnosis for, since there are several stages in this process where problems can occur.
Anything that makes your blood vessels bad at responding to these signals telling them to constrict (like connective tissue diseases) makes it harder for the blood to move to where it needs to go. So, while patients can feel their heart beating faster, they may also feel fatigue or lightheadedness because of lack of blood in the heart and brain.
What is Ehlers-Danlos Syndrome (EDS)?
Ehlers-Danlos Syndrome (EDS), is a genetic disease that causes abnormalities in your connective tissue.
Connective tissue acts to bind, support, or separate your other tissues and organs. Connective tissue is made up of collagen. Collagen is the glue that helps support your bones and make your cartilage and skin flexible. It’s one of the key structural building blocks in your body that helps keep everything together. EDS is caused by a genetic mutation that causes you to lack enough collagen, or weaken it. Because collagen is in your skin, muscles, bones, and blood vessels, this is where the complications occur when you have EDS.
Its effects can be mild or severe. This means that some patients just have particularly flexible joints and skin, while others suffer severe pain and major health complications, like increased risk for internal bleeding or tearing important organ tissues. Having hypermobile joints in and of themselves is not abnormal, but they are a common symptom (accompanied by many others) of EDS.
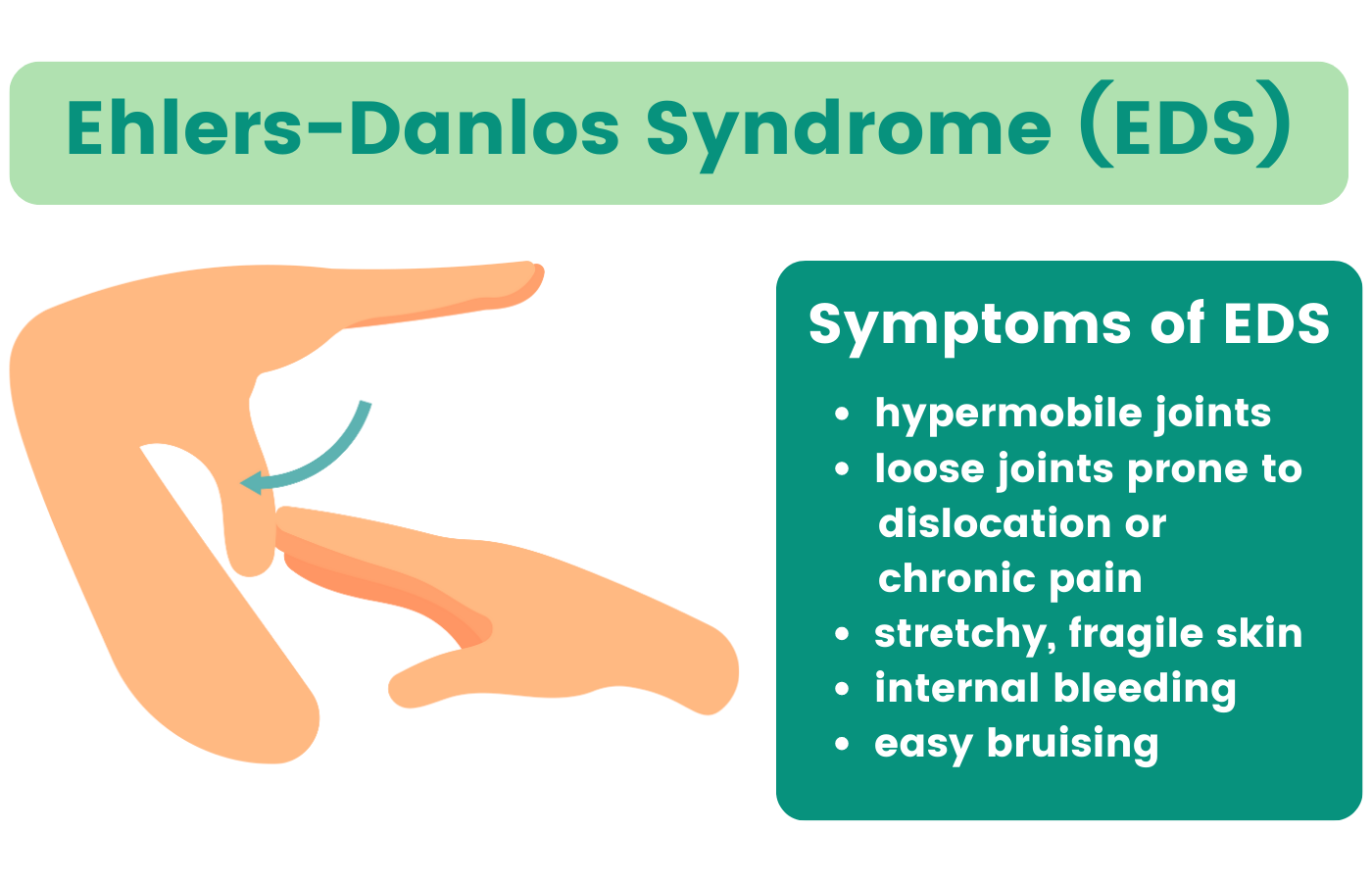
Because EDS is a genetic disease, a large portion of people can actually carry some of the genes for EDS, but only a few have the necessary gene combination for the disease. This makes EDS pretty uncommon. Only about 1 in 5000 people are diagnosed with EDS worldwide (0.02%).
Why Do POTS and EDS Often Occur Together?
As you read above, there are plenty of reasons why someone might have POTS, and by no means does POTS imply EDS. However, there’s enough overlap between the two that it’s worth noting. A small 2017 study, for example, reported that 31% of patients previously diagnosed with POTS satisfied the criteria for also having some form of hypermobile EDS.
A widely accepted (although not thoroughly tested) explanation of why EDS might contribute to POTS has to do with high tissue flexibility. The thinking is that with stretchier tissue around your blood vessels, it’s harder to increase your blood pressure and push fluid upwards. So, your body has to pump out more stress hormones to accomplish the same movement as someone without EDS.
Getting Diagnosed with POTS and EDS

In an interview with our patient ambassador, Liv (aka @chronicallyillandhot) it became abundantly clear that obtaining a proper diagnosis is not an easy feat. So, I asked Liv to walk me through her difficult experience.
1. The Elusive Diagnosis:
Q: Why do you think doctors struggle so much to identify POTS and EDS in their patients?
“I believe it is because connective tissue disorders are not talked about or taken seriously enough in the medical field. Part of that is because of the belief that they’re more rare than they actually are.”
Liv explains that the presumed rarity of these disorders also contributes to the scarcity of research and funding. This slows potential advancements that would be geared toward tools for diagnosis.
Liv also mentioned that the complexity and rarity of these disorders means doctors are typically hesitant to consider them as potential diagnoses, if the doctor has even heard about them before. Unfortunately, it may take lots of time and dead ends before the right diagnosis is reached. If these diseases are not within the doctor’s specialty, they usually are not first to cross their mind in the diagnosis search.
Because your connective tissue supports your joints, bones, surrounding organs, and blood vessels, it is present throughout your entire body. This makes it difficult to target for treatment.
Liv also explained that provider burnout and patient overload limits the amount of time and depth a visit can entail. Limited visit time can mean there may not be enough opportunity to get into all of the nuances of your symptoms and this can make diagnosis even harder. Unfortunately, the combination of provider burnout, patient overbooking, and complex disorders is a recipe for incorrect diagnoses and disheartened patients.
Misdiagnoses may not be completely avoidable, but preparation on your end as the patient may help this process. Ensuring that you are super organized with knowing what you really want your provider to know is really important. Advocate for yourself if you haven’t had your questions answered. Don’t be afraid to schedule follow up visits to get deeper into your symptoms, and make sure you have a provider you feel is really listening to what you are saying.
2. Piecing Together the Puzzle:

Liv also shared some personal experiences that highlight her perseverance in navigating the complex world of medical specialists. She underwent tons of misdiagnoses before finally connecting the right dots.
Q: What type of doctor finally understood your condition and gave you a proper diagnosis?
Before Liv got diagnosed with EDS, she met with specialist after specialist. To name a few, she saw a rheumatologist, an immunologist, a cardiologist, and a neurologist. They all diagnosed her with a myriad of conditions, including rheumatoid arthritis, fibromyalgia, vocal cord dysfunction, mast cell activation syndrome, and finally EDS.
“Finally I saw a gastroenterologist, and this doctor had EDS herself. She was my fifth gastroenterologist in five years.”
Because this specialist also suffers from EDS, she does research about EDS and other hypermobility-related conditions.
“She has helped me more than ANY doctor ever. She did a 2 hour clinical evaluation and made connections I never even considered. Also figured out my GI motility issues in my esophagus and my stomach.”
What Liv and many others with chronic illnesses have experienced, is that it often takes several doctors and oftentimes the kind of doctor you aren’t expecting to finally reach the correct diagnosis. Because doctors are human and imperfect, complex and unusual problems are often quite difficult to diagnose for any doctor. Unfortunately, this is quite a common experience for POTS and EDS patients.
For EDS patients, a 2009 rare diseases study found that 58% of patients saw more than 5 doctors and 20% saw more than 20 doctors before reaching a diagnosis. It was also found that for half of EDS patients, 14 years went by between first experiencing symptoms and getting correctly diagnosed, and 28 years for 25% of patients! For patients with POTS, one survey found that it took an average of four years and seven physicians to reach a proper diagnosis.
3. The Impact of Misdiagnosis:

The same 2009 rare diseases study found that 56% of EDS patients received a misdiagnosis. Receiving treatment for misdiagnoses isn’t something to mess around with. Liv’s been in numerous situations where medications prescribed for incorrect conditions caused her even more health issues.
Q: How have misdiagnoses affected your health, and what advice do you have for avoiding these situations?
“My biggest tip for avoiding misdiagnosis is, honestly you can’t. You can’t help it if a doctor doesn’t know what you have and incorrectly diagnoses you.”
“However, if you have a feeling something isn’t right and don’t feel comfortable going through with treatment, especially when it involves something serious like surgeries, chemo or immunosuppressants, then get a second opinion. No shame in getting a third, fourth or fifth either.”
Before finding her current gastroenterologist (GI), Liv saw four other GIs that offered little to no help and caused even more issues. She had three esophagus dilations, which activated her autoimmune response and made her pain worse.
“The first one... damaged my esophagus after doing three unnecessary surgical procedures in 11 months. I was in so much pain and couldn’t eat anything whatsoever. Even drinking water hurt!”
She was also on low-dose chemotherapy for rheumatoid arthritis (which, if you don’t remember, she doesn’t have).
“Going in low dose chemo absolutely destroyed my gut. I have four gut infections – two fungal and two bacterial that have resisted treatment so far.”
“I also have leaky gut syndrome, that’s apparently ‘as severe as it gets’ according to my doctor... This has improved a lot with treatment, but I have to pay out of pocket for that treatment.”
Leaky gut syndrome has to do with the permeability of your gut intestines. Different factors like stress, unhealthy diet, drugs, alcohol consumption (and in Liv’s case, chemotherapy) all can compromise the barrier walls of your intestines. The health of your gut microbiome also contributes to how well that barrier can absorb the good nutrients and block out toxins (like bad bacteria) from entering your bloodstream. When these harmful substances leak in, your immune response increases, and inflammation increases. People with EDS have higher susceptibility to gut permeability because having hyper flexible connective tissue could cause their intestines to be more permeable.
4. Empowerment through Patient Communities:
Liv expressed immense gratitude for the support she receives from online patient communities, especially through social media platforms like TikTok and Facebook groups. They do a good job of providing educational content while also connecting those who understand the challenges of living with POTS and EDS.
Q: How have online patient communities helped you on your health journey, and what benefits do they bring to individuals facing similar challenges?
“Tiktok helped me figure out what was actually wrong through all the educational content, and led me to websites where I could find research papers.”
A friend of Liv’s who is a professor granted her access to research papers on all things EDS and connective tissue disorders. After learning more about her newly diagnosed condition, she was able to seek helpful support.
“That led me to Facebook support groups, where I learned a lot from Q & A’s! The only thing is they kind of aren’t “support” groups, as sometimes people just are not always kind on them. But those groups, the local ones, helped me find some EDS aware doctors!”
Liv, desiring to foster a more positive and uplifting community, decided to create a group of her own.
“I created a discord chronic illness group with around 500 members last I checked. Though I’m not in it as much as I’d like, every time I need some advice or to vent about my conditions, everyone is SO helpful and supportive. Literally the best group of people on there imaginable.”
5. Building a Supportive Network:

While online communities offer valuable support, real-life interactions can make a significant difference. However, achieving greater accessibility and understanding in local communities remains a challenge.
Q: In what ways do you believe real-life support networks can be improved to better accommodate individuals with POTS and EDS?
“Real life support, well we need things to be more accessible. It would be nice if more people were understanding of our limitations.” (edited)
Basically, the availability of in-person support networks increases when awareness and compassion increase for those with POTS and EDS.
The Bottom Line
The road to diagnosis and support for POTS and EDS can be difficult, but the journey is evolving with the emergence of health tech start-ups and growing online and in-person supportive patient communities. The need for better awareness, funding, and research is necessary to bridge the resource gap and improve the lives of those navigating these complex conditions. As awareness spreads, hope and empowerment will become more accessible to all who face the challenges of POTS and EDS.