We all know the age-old line your parents have used after you've bartered for another piece of cake or scoop of ice cream: "Sugar is bad for you." It seems unquestionable with sugar-free versions of drinks and dessert almost as common as the original ones. But is this really true? Can something that tastes so good be just so bad? In hopes of raising your spirits, I will say sugar is essential. Our bodies cannot live without it. But to bring us back to reality… too much sugar can be quite a problem.
Massive amounts of sugar can contribute to a rise in our blood sugar and all kinds of detrimental complications. You may think there’s an obvious way to manage it: eat less dessert and more vegetables. But it's not that simple. To learn how to prevent these risks, we must first understand what blood sugar is, how it changes, and why it's so important to pay attention to it.

So what exactly is blood sugar?
Blood sugar or blood glucose refers to the level of glucose found in your bloodstream at that moment. Glucose is a sugar that serves as our primary energy source. Our body obtains glucose from our food and carries it through the bloodstream to our cells. Our cells then break down glucose and convert it into energy.
One of the key players in managing your blood sugar levels is insulin. Insulin is a hormone produced by your pancreas. It aids in transporting glucose from your bloodstream into your cells. A mostly impenetrable barrier surrounds your cells as protection, but within the barrier, there are "doors" (known as channels) for glucose to enter through. Insulin acts like a key to these channels, "unlocking" or opening them to allow glucose to flood into the cell. However, if you have low insulin levels or ineffective insulin, glucose is forced to accumulate in the bloodstream, creating a rise in your blood sugar.
Well, why does it matter so much?
Even though glucose is always present in your blood, significantly high or low blood glucose levels can lead to complications.
If your blood glucose is too high, it can cause complications like heart disease, stroke, kidney disease, and more. High blood sugar can also cause type 2 diabetes. Type 2 diabetes is the most common form of diabetes, and those with a family history of this disease or who are overweight/obese are particularly at risk.
Type 2 diabetes can occur from insulin resistance, a condition where your cells stop responding to insulin as effectively as they should. This concept is similar to caffeine tolerance. At first, those morning cups of Joe keep you bright-eyed and bushy-tailed through all your early meetings. And it does for a little, until you begin to feel less and less energized. Suddenly, your one cup turns into two or maybe three throughout the day. But what you don't realize is that your overcompensation of coffee consumption is actually creating a tolerance, meaning your body is responding less and less to its caffeinating effects.
In a similar way, if an influx of glucose enters your body from a high-sugar meal, your pancreas must release more insulin. However, over time, a high level of insulin production creates a weaker response from your cells. Glucose is then "locked out" of your cells and instead accumulates in your bloodstream.
Well, can’t I just eat better? Do I really need to track it?

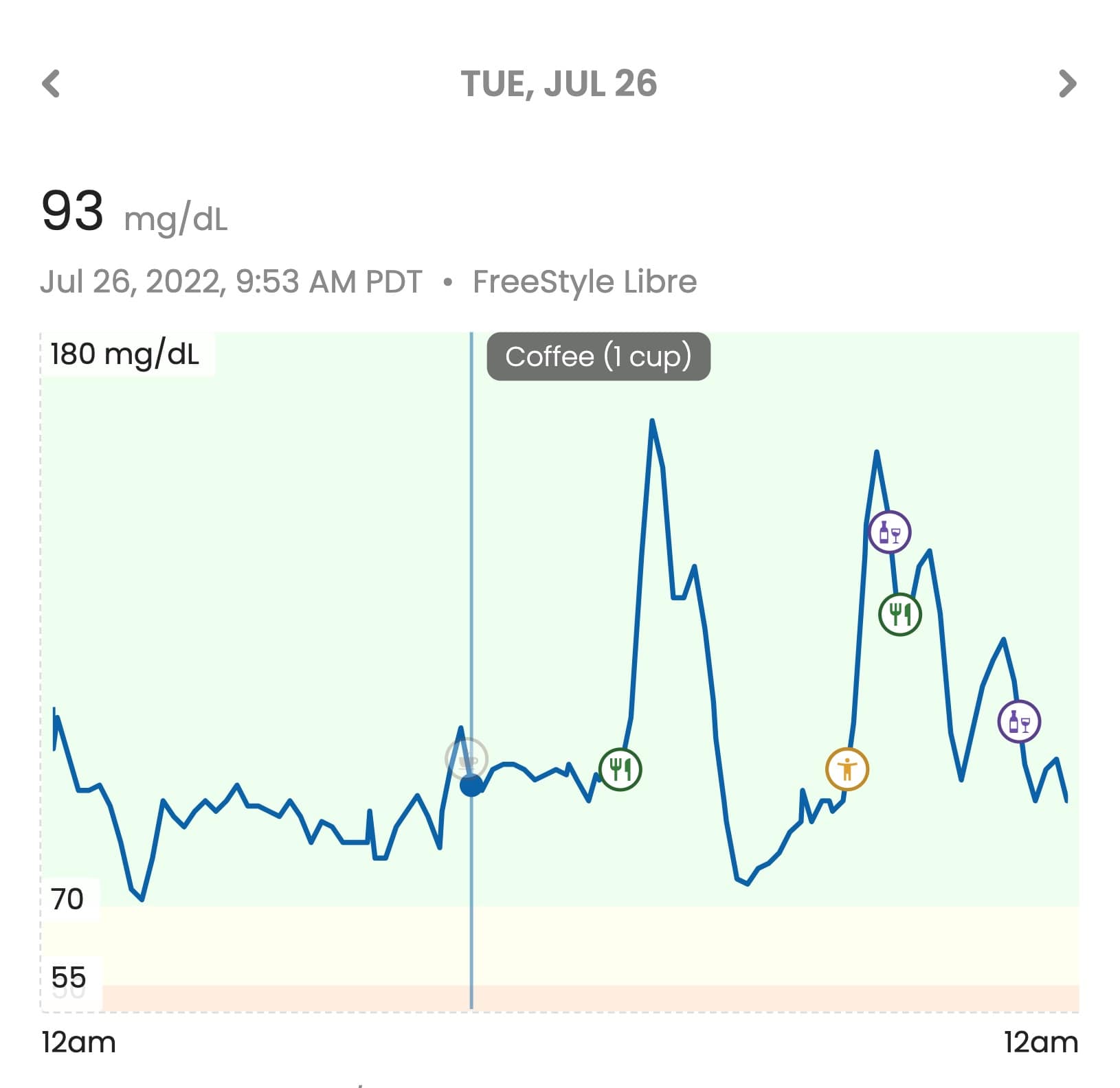
One important reason to monitor your own blood glucose is that everyone’s blood sugar responds differently to things like food, diet, stress, and more.
Generally speaking, a healthy diet, such as eating more vegetables and consuming fewer calories, can improve your blood sugar. Nonetheless, most of us categorize granola bars as a healthier option than cupcakes, but it’s quite possible a granola bar can cause a higher spike in blood sugar for you specifically.
In the same way, exercise often lowers your blood sugar levels and can increase your insulin efficiency. Yet, sometimes you can see a rise in blood sugar, especially during high-intensity workouts. This is normal and is due to an increase in adrenaline. The hormone adrenaline signals the release of glucose that's been stored in your liver to serve as extra fuel. But even so, a spike during exercise or a meal may not be ideal for those trying to keep their blood sugar in a very specific range.
To summarize, you can’t effectively manage your blood glucose response with generalized advice. To truly understand how to lower it, you must understand what naturally lowers or raises your own blood sugar levels. Logging how your levels react to certain foods or exercises or medications can help you get a better picture. Paying attention to your own body’s response allows a more valuable and personalized lifestyle than one you can find on the internet.
Ok, I’m convinced. Now, how can I track my blood sugar?
1. Glucose Monitors
An essential part of managing your blood sugar is measuring it. Technology has made this process more accessible than ever before with the creation of continuous glucose monitors (CGMs). These devices work by inserting sensors under your skin, allowing the CGM to monitor your glucose levels every few minutes. Companies such as Dexcom and Abbott (who make the FreeStyle Libre) create CGMs. These CGMs are compatible with smartphone apps that display readings, show correlations, and provide a deeper understanding of your own blood sugar management. This technology is a valuable tool to improve your blood glucose levels past the general recommendations.
2. Blood Glucose Testing
Another way to monitor your blood sugar is through medical testing. There are four tests you can receive: the A1C test, the Fasting Blood Sugar Test, the Glucose Tolerance Test, and the Random Blood Sugar Test.
The A1C test estimates your blood glucose levels in the last 3 months. The other three tests measure your blood glucose at that moment. Because blood sugar can change significantly after eating or drinking, the Fasting Blood Sugar Test and the Glucose Tolerance Test depend on when your last meal was. The Fasting Blood Sugar Test measures your blood sugar after fasting for at least 8 hours. On the other hand, the Glucose Tolerance Test measures your levels 2 hours after a meal. Therefore, the results of these tests are quite different. Lastly, the Random Blood Sugar Test can be done at any time and diagnoses those with over 200 mg/dL as diabetic.
The CDC's values are often used when testing for diabetes or prediabetes, but several studies have shown that a healthy blood sugar level may be lower than the CDC's recommendations.
| Normal | Prediabetic | Diabetic | |
|---|---|---|---|
| A1C Test | < 5.7 % | 5.7-6.4 % | ≥ 6.5 % |
| Fasting Blood Sugar Test | ≤ 99 mg/dL | 100-125 mg/dL | ≥ 126 mg/dL |
| Glucose Tolerance Test | ≤ 140 mg/dL | 140-199 mg/dL | ≥ 200 mg/dL |
| Random Blood Sugar Test | N/A | N/A | ≥ 200 mg/dL |
Even though blood sugar levels below 140 mg/dL are considered normal, levels below 70 mg/dL are considered low and can have serious complications if left untreated. If you believe you could be at risk of high or low blood sugar, talk to your doctor about which test might be right for you.

Diabetes is a lot more common than you may think. This year the CDC estimated that more than 130 million adults are diabetic or prediabetic in the US. It is also the eighth leading cause of death for Americans and cost the United States around $327 billion in 2017.
Talk to a healthcare professional if you think you could be at risk. Proactivity is one of the most effective ways to stop the development of this incurable disease. Don’t condemn yourself to a life of insulin pumps, pills, and medical bills.