When it comes to food-related health issues, it's easy to get confused between food sensitivities and food allergies. Despite the symptoms of both conditions being similar, they're different in terms of their causes and severity.
While eating food you are intolerant to can cause discomfort and leave you feeling sluggish, eating food you are allergic to can be life-threatening. Understanding these differences is important when it comes to managing your health and knowing when to seek professional help.
What Are Food Sensitivities?
Food sensitivities, also known as food intolerances, are non-immunological responses that occur when your body reacts abnormally to certain foods and has a difficult time digesting them. Common food sensitivities include:
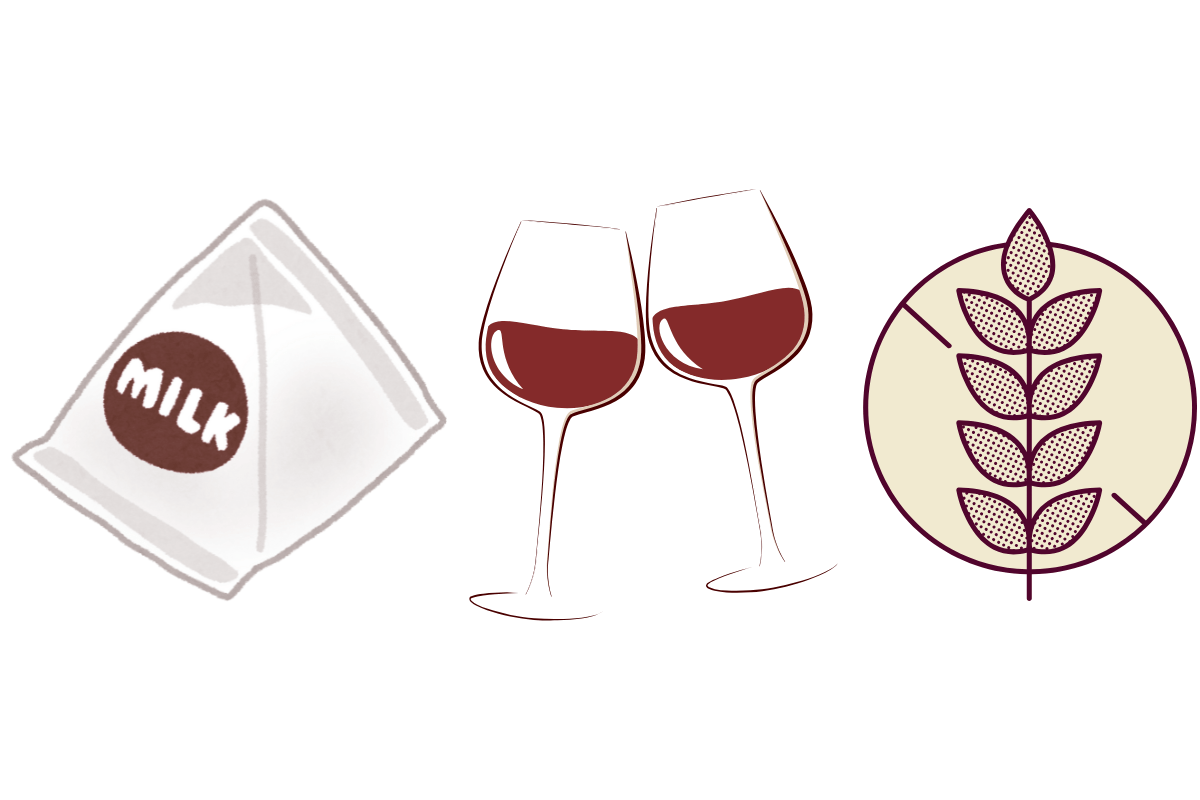
Lactose:
This occurs in people who don’t have sufficient lactase, an enzyme that breaks down lactose, or a type of sugar found in dairy products. When lactose isn’t properly digested, it can lead to symptoms like bloating, diarrhea, and gas as the undigested lactose ferments in the colon.
This is why people with lactose intolerance can manage their symptoms by avoiding dairy or using lactase supplements to aid digestion.
Histamine:
This is a molecule that is naturally present in foods like dried or preserved fish, cheese, avocados, and wine. Some people don’t produce enough diamine oxidase–an enzyme that breaks down histamine–and are therefore intolerant to foods containing the chemical. When histamine builds up in the body, it can trigger symptoms like headaches, skin rashes, hives, nasal congestion, and digestive issues.
Gluten:
This is a protein found in wheat, rye, and barley. There are three primary ways people can react to gluten: gluten intolerance, gluten allergy, and celiac disease, but only gluten intolerance can be classified as food sensitivity.
Gluten intolerance is when people experience intestinal symptoms like discomfort or bloating after consuming gluten, but it doesn't cause permanent damage to the digestive tract. This is the most common gluten-related condition out of the 3 mentioned, affecting up to 13% of the general population.
The exact causes of gluten intolerance are not well understood, but some studies suggest that wheat can affect the lining of the digestive tract. This lining usually prevents harmful bacteria from entering the bloodstream. However, in those with gluten intolerance, this barrier can break down, allowing bacteria to enter and cause inflammation.
Understanding the differences between these conditions is key to identifying the right course of action for treatment.
Some Symptoms of Food Sensitivities
The symptoms of food sensitivities are usually less severe than allergies, but they can still affect your day-to-day life, and they may appear hours or even days after eating the trigger food. These sensitivities are often chronic, meaning they may persist long-term. People typically manage this by eliminating the foods that trigger their intolerance.
- Bloating and gas
- Stomach cramps or pain
- Nausea or diarrhea
- Fatigue
- Headaches
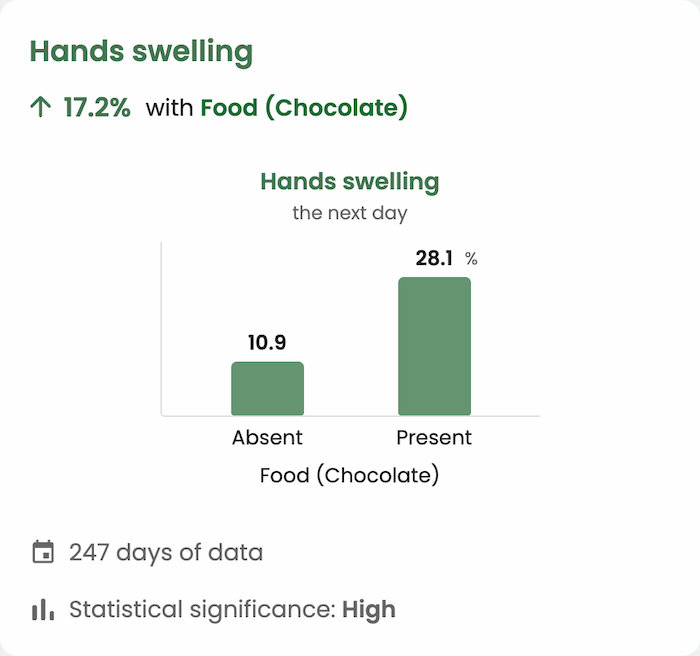
With Guava, you can track your food intake and symptoms, allowing you to recognize potential intolerances and develop a personalized approach to your diet.
Testing & Diagnosis:
Diagnosing food sensitivities can be challenging because the symptoms do not always occur immediately and are usually more varied than those of food allergies. If you suspect you have a food sensitivity, working with a healthcare professional to get a diagnosis can help you learn ways to manage your symptoms and avoid flare-ups.

Not only will testing help your body avoid physical discomfort, but for many, knowing what’s happening inside their body can provide a sense of relief and peace of mind. With this knowledge, you can be better equipped to take control of your diet and feel less worried about potential unidentified triggers and unexplained symptoms. Here are a few common testing methods for food allergies:
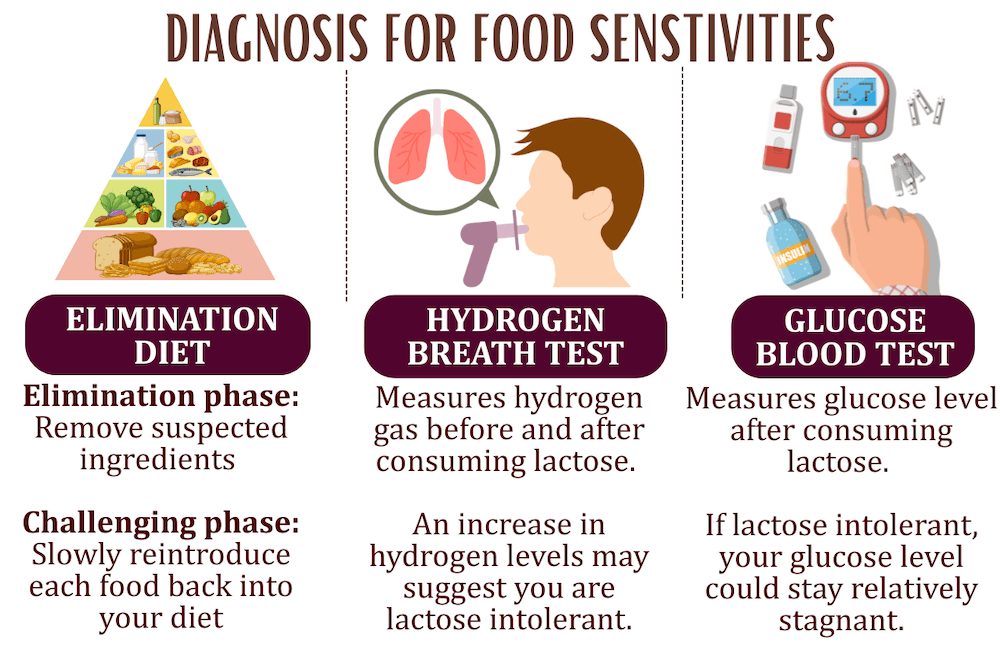
Elimination diet:
An elimination diet is a meal plan that removes certain groups or ingredients to find which foods may cause sensitivity.
This method begins with an elimination phase, where you remove the food you suspect is causing you discomfort. It’s important to read food labels carefully, be aware of the ingredients used in dishes at restaurants, and track everything you eat and your responses to it. This phase typically lasts around 3 weeks.
The next phase is the challenging phase. Once you have eliminated potential food triggers, you can slowly reintroduce each food back into your diet, one at a time. You should keep a buffer of 3 days each time you add a new food to provide your body time to react.
During this testing period, you may want to track all your reactions and symptoms. With Guava, you can easily monitor and record your body responses, making it easier to track your progress and pinpoint any food sensitivities.
Blood or Breath Tests (i.e. Lactose Tolerance Test):
The lactose tolerance test examines whether your body can break down lactose when consuming milk, cheese, and dairy products. There are two types of lactose tolerance tests:
Hydrogen Breath Test:
This test tracks the amount of hydrogen in your breath before and after consuming a lactose-containing liquid. If your body is unable to fully digest the lactose, it will be broken down by bacteria in the large intestine. This creates hydrogen gas, which you breathe out. An increased level of hydrogen may suggest you are lactose intolerant, but it’s important to consult a healthcare professional for a proper diagnosis and further guidance.
Glucose Blood Test:
This method measures your blood glucose levels before and after consuming a lactose-containing liquid. If you're lactose intolerant, you might not experience a significant rise in blood glucose levels, as your body has a hard time breaking down lactose into lactase. When lactose isn't properly broken down, less glucose is absorbed into the bloodstream.
For these tests, your healthcare professional may ask you to fast for eight to 12 hours beforehand, stop taking antibiotics for two to four weeks before, and/or refrain from smoking or exercising the day before the test. These measures may help create an accurate baseline evaluation of your blood glucose or hydrogen levels without interference from recently consumed food, drinks, or antibiotics that may affect your gut bacteria.
Management & Treatment for Food Sensitivities
The most straightforward way to manage food sensitivities is to alter your diet and eliminate foods that upset your digestion. When you do react to food intolerances, over-the-counter medicines such as antacids can help relieve uncomfortable symptoms caused by indigestion.
Those who are lactose intolerant may also use lactose-free milk, such as non-dairy milk, or dairy milk that has been treated. There are several ways to make dairy milk lactose-free, so it may take some experimentation to find the option that works best for you. You can also try consuming lactase enzymes in the form of a pill or liquid drop directly before consuming dairy to help break down the lactose.
What Are Food Allergies?
Unlike food sensitivities, allergies involve the immune system, where the body mistakenly identifies a harmless food as a threat and triggers an immune response. The body produces immunoglobulin E (IgE) antibodies, which can result in allergic reactions that may be life-threatening.
As mentioned earlier, gluten can trigger three main types of reactions, one of which is an allergic reaction. A gluten allergy can cause symptoms such as hives, swelling, and difficulty breathing.
Other common food allergens are:
- Peanuts
- Shellfish
- Milk
- Soy
- Eggs
- Fish
Common Symptoms of Food Allergies
- Hives, itching, swelling (common around the face and lips)
- Difficulty breathing or shortness of breath
- Abdominal pain, nausea, or vomiting
- Dizziness or fainting
The symptoms of food allergies are usually very intense and occur immediately, within minutes to an hour of eating the allergen. Due to the severe reactions of certain responses like anaphylaxis, food allergies require strict avoidance of the allergenic food and may demand immediate medical attention upon exposure.
Testing & Diagnosis for Food Allergies
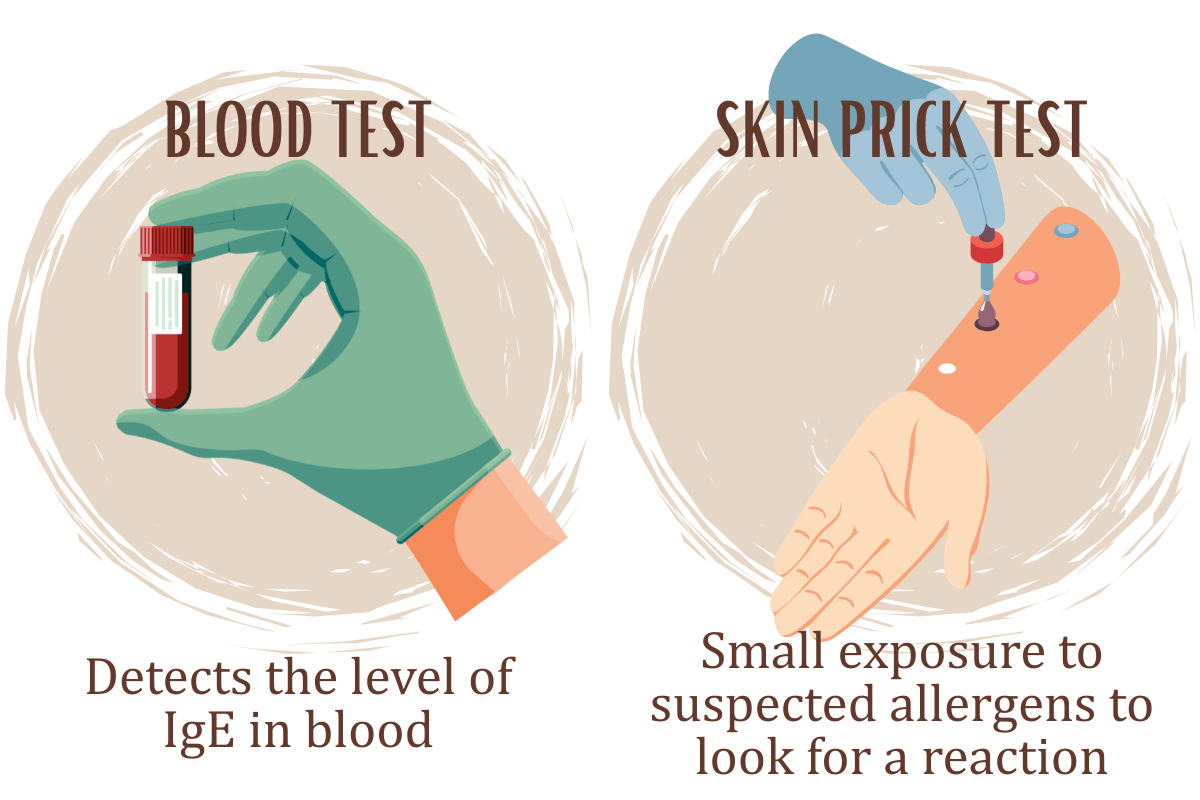
Food allergies are generally more straightforward than food sensitivities and can be determined using a skin prick test or blood tests that reveal IgE levels for certain allergens.
Skin prick test:
During the skin prick test, the skin is exposed to suspected allergens to determine if you will react to them. Although skin tests are typically safe for everyone, your healthcare provider may recommend against them if you have had a severe allergic reaction in the past. Your healthcare provider may also recommend other testing methods if you are on certain medications, like antihistamines, as they can interfere with the results or if you have specific skin conditions like eczema or urticaria that affect the coloring on areas of your skin.
Blood test:
An allergy blood test measures the level of Immunoglobulin E (IgE) antibodies in your blood. IgE is a type of protein produced by the immune system in response to allergens. When the body mistakenly identifies a harmless substance as a threat, it releases IgE, which triggers an allergic reaction. Generally, you don’t need to prepare anything in advance. After the test is finished, you will receive a scoring system that shows how serious your allergy is.
Management & Treatment for Food Allergies
Avoiding foods you are allergic to is the best management option. Sometimes, if certain common allergens are difficult to avoid, your healthcare provider may recommend daily medications to reduce symptoms or the risk of a reaction. This includes:
Antihistamine:
Antihistamines are medications that work by blocking the effects of histamine, a chemical released by the immune system during an allergic reaction. When histamine binds to certain receptors in the body, it causes symptoms like sneezing, itching, runny nose, and watery eyes. By preventing histamine from attaching to these receptors, antihistamines reduce or eliminate these common allergic symptoms, like fever, seasonal allergies, or allergic reactions.
Steroid Nasal Spray
Steroid nasal sprays reduce inflammation by delivering a corticosteroid to the nasal passages. Corticosteroids are medications that replicate the natural steroid hormones produced by the body, which can suppress inflammatory chemicals and reduce the activity of immune cells.
Leukotriene Modifiers:
Leukotriene modifiers are medications that block the release of leukotrienes, which are chemicals produced by immune cells in response to an allergic reaction. These chemicals contribute to inflammation and swelling of the airways, leading to symptoms like shortness of breath or congestion. By blocking the release of leukotrienes, these medications help reduce inflammation, making them useful for managing allergic reactions.
Omalizumab (Xolair) injections:
Omalizumab (Xolair) injections are the most widely used allergy treatment in the United States. Omalizumab is an antibody that targets and neutralizes IgE antibodies, preventing them from binding to immune cells and triggering an allergic response.
Allergy Shots (Immunotherapy):
Allergy shots involve receiving small, controlled doses of the allergen you’re allergic to, typically administered in a medical setting by a trained healthcare professional. Over time, the dose of the allergen is gradually increased. This process helps your immune system become less sensitive to the allergen, reducing the severity of allergic reactions.
It’s important to understand that allergy shots are generally administered by a doctor or trained allergist, as they monitor the process for any potential adverse reactions. Administering allergy shots on your own at home is not recommended due to the risk of complications or improper dosing. Regular visits to your healthcare provider are often necessary to ensure the treatment is both safe and effective.
Sublingual immunotherapy (SLIT):
This is similar to allergy shots, but SLIT is taken in tablet or drop form.
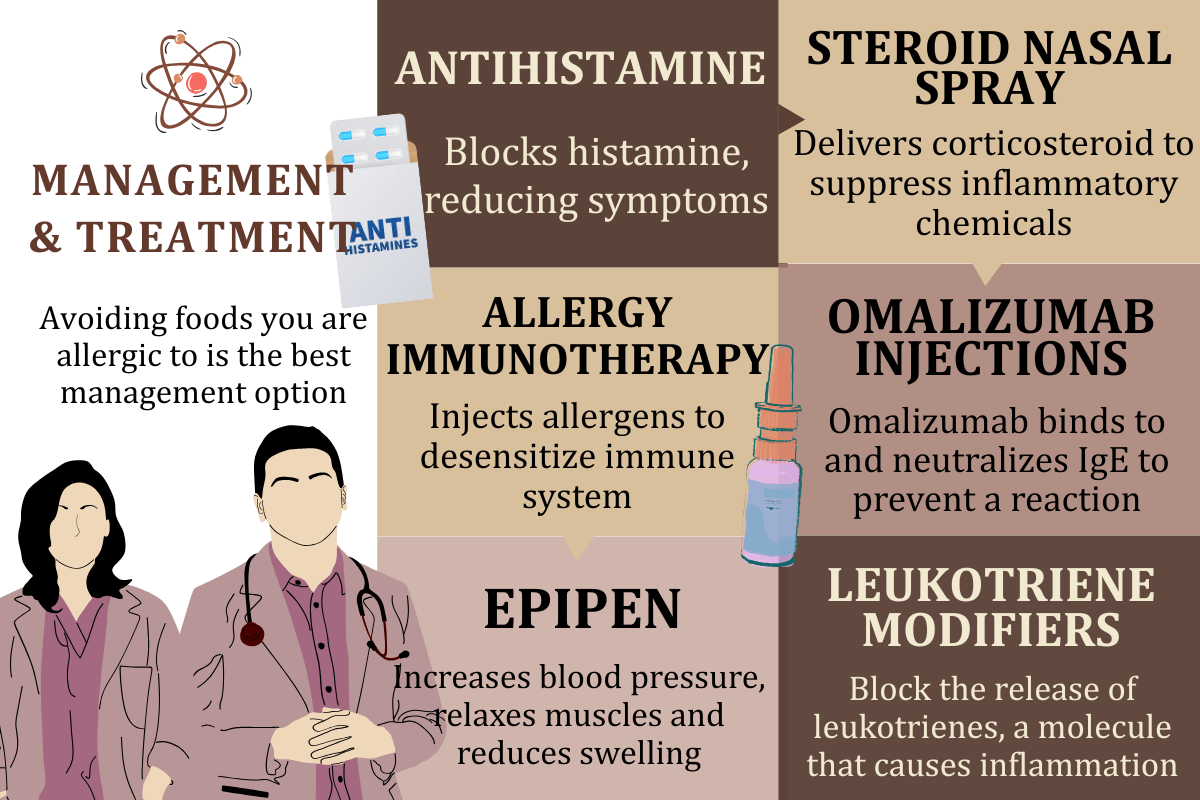
A healthcare provider may also suggest carrying an epinephrine auto-injector (EpiPen or Auvi-Q) at signs of a severe allergic reaction. These devices are designed to quickly deliver a dose of epinephrine (adrenaline) to counteract the life-threatening symptoms of anaphylaxis.
Epinephrine is a hormone that helps raise blood pressure, reduce swelling, and open airways during an allergic reaction. It’s easy to use and can be administered by the person having the reaction or by someone else in an emergency.
A reminder from Guava’s Chief Medical Officer, Dr. Kat McGraw MD: It’s important to check the expiration date of your EpiPen or Auvi-Q regularly, as they can lose effectiveness over time. People frequently carry it around for years and may not realize they are expired when they need it most.
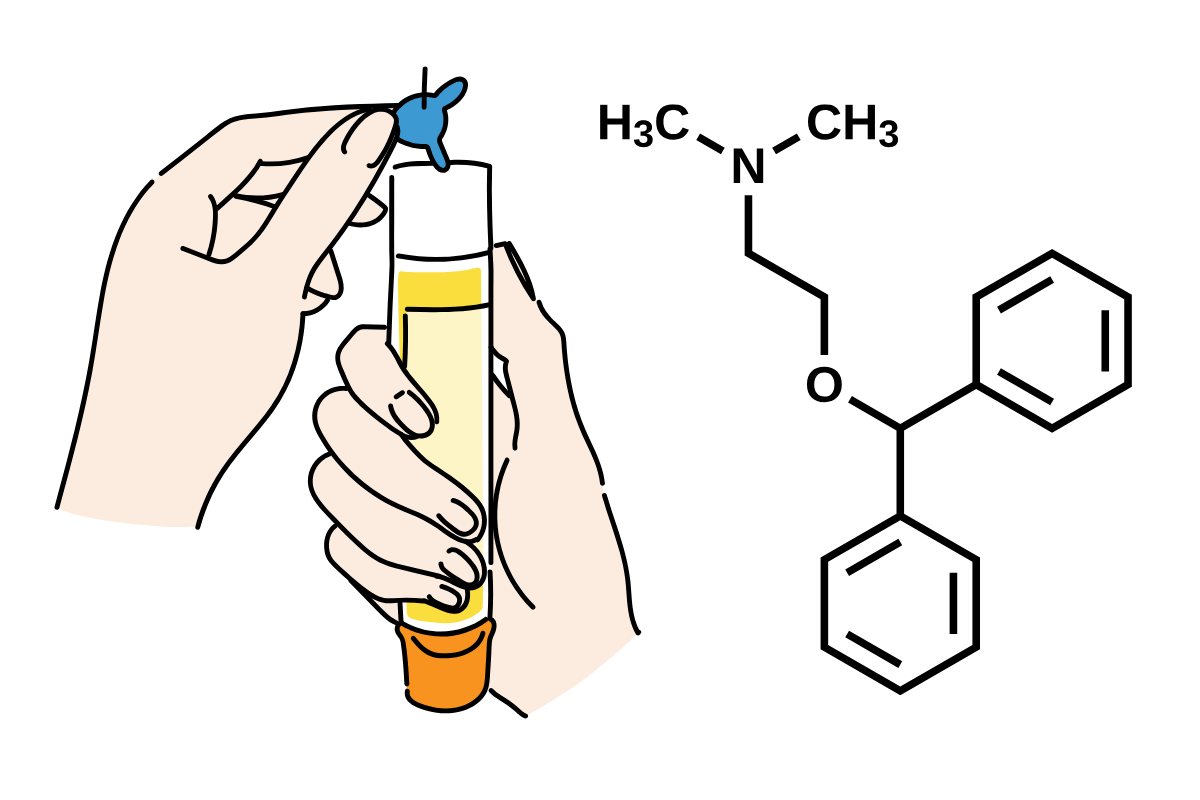
In addition to an EpiPen, Benadryl (diphenhydramine) tablets can help with milder symptoms like sneezing, itching, or hives by blocking the effects of histamine. However, it may not be effective for severe allergic reactions like anaphylaxis so it can be useful to also have an EpiPen on hand at all times.
Furthermore, it is important to call 911 for emergency care if you experience extreme discomfort, such as chest pain, tingling hands, feet, or lips, difficulty breathing, or more.
Being aware of your food allergies and having treatment options ready can also be useful self-care and coping mechanisms. In addition to medical interventions, stress management techniques like mindfulness, meditation, and regular exercise can also reduce anxiety related to allergies.
Tracking your symptoms and triggers with food using Guava can help you maintain an accurate record of your allergic reactions, providing insights into how you can better manage your health.
Can You Have Both Food Allergies and Sensitivities?
It is possible to have both food allergies and sensitivities. Some people may be allergic to certain products and also experience digestive issues with others. Managing both conditions requires careful attention to your eating patterns, and seeking advice from a healthcare provider is recommended.
Conclusion
While food sensitivities and food allergies are both conditions related to food, they differ in many ways and have different extents of severity. If you suspect that you have either of these conditions, it could be a good idea to consult with a healthcare professional for proper management strategies.
Track Your Reactions to Food with Guava
If you're experiencing symptoms, tracking them with Guava can help you and your provider spot patterns and tailor a treatment plan. You can monitor heart rate, digestion, and food responses—all in one place—and easily share the data with your care team.