If you’re someone who menstruates, then you’ve more than likely experienced your fair share of days when a persistent ache in your lower abdomen seemed to demand your attention and caused considerable discomfort. This sensation is a natural part of the menstrual cycle that people everywhere who experience periods are familiar with. In this article, we're going to dive into the science behind what causes these uncomfortable pains and share some ways to make them more manageable.
If you’re curious about periods and how the whole menstrual cycle works, give this guide to periods a read!
What are Menstrual Cramps?
Menstrual cramps refer to the painful sensations that occur in the lower abdomen before and during menstruation. They are typically characterized by recurrent contractions of the uterus, which help expel its lining. The severity of menstrual cramps can vary from person to person, with some experiencing mild discomfort while others may experience debilitating pain.
However, when these cramps become severe enough to require medical attention, it is referred to as dysmenorrhea. Dysmenorrhea can occur before or during a period and persist throughout the menstrual cycle. 84.1% of people who menstruate face some level of period-related discomfort, and approximately 31.9% of those with dysmenorrhea even miss school or work due to the severity of the pain according to this NIH study, though these numbers are suspected by healthcare providers to be higher as individuals may not report menstrual pain.

Causes of Menstrual Cramps
Each menstrual cycle, except during pregnancy, the uterine lining goes through a cycle of buildup and shedding. This shedding occurs through irregular muscle contractions in the uterus, allowing the lining and blood to be expelled through the cervix and vagina. While these contractions may be unnoticed or mildly uncomfortable, they can also lead to painful cramps felt primarily in the lower abdomen, back, or legs.
Specifically, the NIH indicated that these cramps are due to the release of prostaglandins, which act like messengers in your body to help control pain and inflammation. When the lining of the uterus breaks down and sheds during menstruation, prostaglandins are released, causing the uterine muscles to contract. These contractions are what lead to the familiar cramping sensation.
Types of Dysmenorrhea
Dysmenorrhea can be categorized into two main types: primary and secondary.
Primary Dysmenorrhea
Primary dysmenorrhea is the most common form of menstrual cramps and is not caused by any underlying medical condition. The pain is often crampy and occurs in the lower abdomen. It may be accompanied by other symptoms such as headache, nausea, diarrhea, and fatigue. Research indicates this typically begins within 6 months to two years of a person's first period and is most severe within the first 72 hours of menstruation.
Secondary Dysmenorrhea
On the other hand, secondary dysmenorrhea is caused by underlying reproductive system disorders such as endometriosis or fibroids, resulting in longer-lasting and more persistent pain. In fact, it’s estimated that about 3 in 10 people who experience dysmenorrhea may have endometriosis.
Secondary dysmenorrhea may present with more severe pain that is localized in a specific area or radiates to the lower back. The pain may also be accompanied by heavy or irregular menstrual bleeding, pelvic pain outside of menstruation, and other symptoms related to the underlying medical condition.

Secondary Dysmenorrhea and Underlying Conditions
The American College of Obstetricians and Gynecologists indicates that secondary dysmenorrhea is often linked to conditions like endometriosis or ovarian cysts. These conditions can result in ongoing discomfort and pain exceeding that caused by the menstrual period.
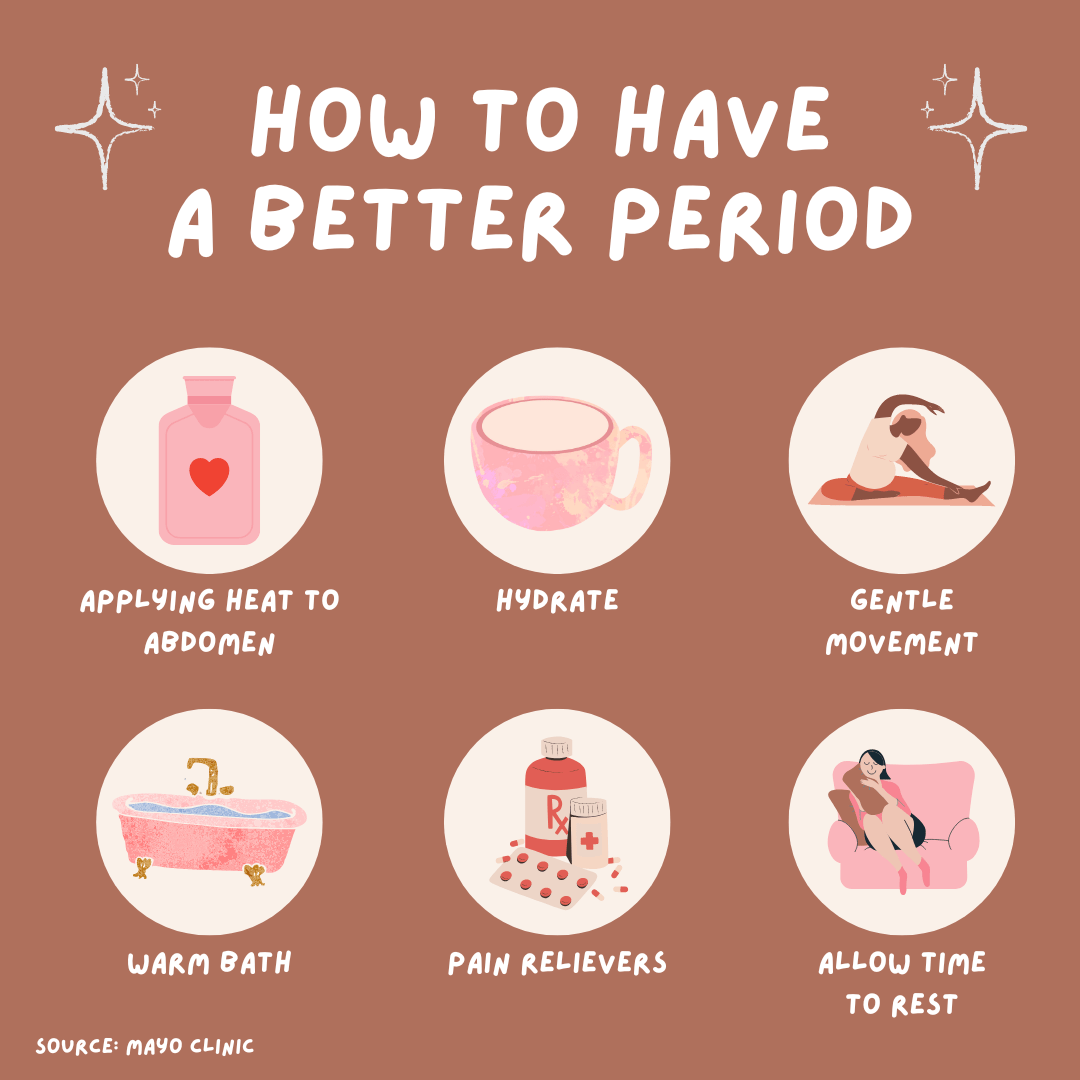
Management
The NIH suggests treatment options for menstrual cramps involving a combination of lifestyle changes, over-the-counter pain relievers, and hormonal medications. Applying heat to the abdomen, taking warm baths, and practicing relaxation techniques can help alleviate pain and discomfort. In some cases, healthcare providers may recommend prescription medications or surgical interventions to manage severe or persistent menstrual cramps.
Note that while these methods can be helpful, there is currently a shortage of comprehensive scientific studies to fully support their effectiveness. Additionally, each individual experiences menstruation differently, and trying out these various approaches might lead to different outcomes.
If menstrual cramps significantly disrupt your daily life or you notice worsening symptoms over time, consult a healthcare professional for an accurate diagnosis and appropriate treatment plan. Don't hesitate to seek medical attention for your menstrual cramps—whether you're uncertain about your symptoms or worried they might be dismissed. Remember, seeking medical advice is completely valid and crucial for your well-being. If you're concerned about your symptoms being taken seriously, this article about bias in pain perception offers valuable advice on effectively communicating your health concerns in medical settings.