You have probably experienced this exact scenario: sitting with your girlfriends, sharing stories about your day, when suddenly the conversation turns to stomach troubles. From bloating and discomfort to unpredictable bowel movements, it seems like many of us experience gastrointestinal (GI) issues on a regular basis. But what exactly causes these problems?
Let’s explore some of the most common abdominal problems that you may encounter, and understand what hormonal and alternative factors may be contributing to these all-too-common complaints.
5 Common Abdominal Problems You May Encounter As a Woman
1. Bloating
What is bloating?
Bloating is a sensation that many of us are all too familiar with, and research reveals that women are more than twice as likely to report feeling bloating than men. Bloating is a sensation of tightness or swelling in your abdomen, ranging from mild discomfort to severe pain.
It is also important to note that bloating is not always accompanied by a visibly swollen abdomen. This is significant because if you, or even healthcare professionals, only focus on visible signs of bloating, the seriousness of the symptoms may be dismissed, delaying proper treatment.
What causes bloating?
The most common cause of bloating is excess intestinal gas, which can be caused by factors like eating too much too quickly or having a food intolerance. When you eat large quantities of food rapidly, your stomach becomes distended as it fills with food. This can lead to a feeling of fullness and discomfort, which manifests as bloating. Eating quickly can also cause you to swallow more air, leading to increased gas in the digestive system, further exacerbating bloating.
Additionally, certain individuals have difficulty digesting specific foods due to a lack of certain enzymes or sensitivity to certain components. For example, lactose intolerance, where the body lacks the enzyme lactase to digest lactose (the sugar in milk), can lead to gas production and bloating.
These problems might be more specific for women because studies show that women may be more susceptible to certain dietary triggers than men. Changes in gut microbiota and immune system differences between men and women contribute to these intolerances and sensitivities.
In terms of menstrual factors, it's not uncommon for you to feel bloated before your period, and for some, this sensation continues into the early stages of menstruation. Menstrual bloating is associated with fluctuations in estrogen and progesterone levels, leading to increased water and salt retention. Around 75% of women experience bloating before or during their period.
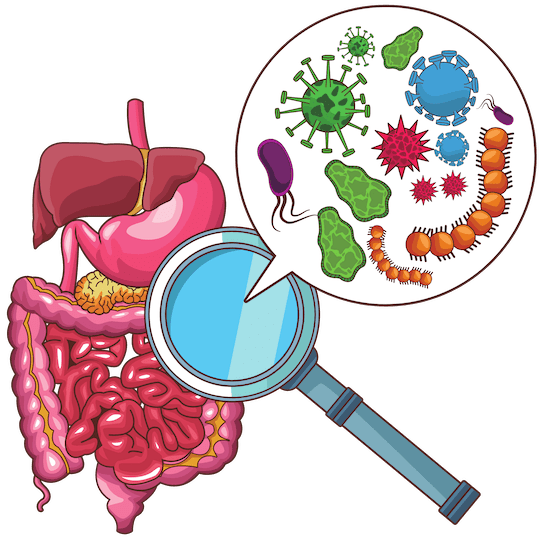
Another cause of bloating can be bacterial overgrowth. This occurs when there is too much normal bacteria in the small intestine.

- How do you know if you have it? Bacterial overgrowth can cause various gastrointestinal symptoms, including bloating, abdominal pain, gas, diarrhea, and sometimes weight loss. These symptoms can be similar to those of other GI conditions, which makes it essential to speak to a healthcare professional for an accurate diagnosis. Advanced age and immunodeficiency disorders might contribute to overgrowth.
- How can normal bacteria be a problem? While normal bacteria play a vital role in maintaining a healthy digestive system, their overgrowth in the small intestine can lead to the fermentation of undigested carbohydrates, producing excess gas and causing symptoms like bloating and discomfort.
- Is it dangerous? Bacterial overgrowth is not usually life-threatening, but it can significantly impact a person's quality of life and cause significant discomfort and distress. If left untreated, it can lead to malabsorption of nutrients, which may result in nutritional deficiencies and unintended weight loss.
- Will it cause infections? How would I know? Bacterial overgrowth itself is not an infection, but it can lead to symptoms and complications that mimic infection or other gastrointestinal disorders. If you are unsure about your symptoms or if they worsen or persist, it's essential to consult a healthcare professional for a proper evaluation and diagnosis.
- How common is it? While the exact prevalence can vary depending on the population studied and the diagnostic criteria used, it is considered to be a relatively common condition. Doctors also assume that bacterial overgrowth is generally underdiagnosed.
If your bloating doesn’t go away or keeps getting worse, you should seek medical attention.
2. Irritable Bowel Syndrome (IBS)
What is IBS?
IBS is one of the most common GI disorders and is defined by abnormal bowel movements with no detectable disease, as well as abdominal pain. IBS is a chronic condition that can last years.
IBS can be recognized by four main symptoms: diarrhea, constipation, abdominal discomfort, and alternating loose stools. Some other notable symptoms include mucus in stool and the feeling that a bowel movement has not been complete even if it has.
What causes IBS?
The exact causes of IBS remain unknown. While the condition seems to be more common among women and individuals under 50 years of age, the precise reasons for its development are not fully understood.
Notably, IBS symptoms might intensify during the menstrual period, but it's important to clarify that the period itself is not the root cause of IBS. Fluctuating hormone levels have a strong impact on the GI system, which can make symptoms more severe. One study found that more than 50% of women with IBS have worse symptoms before or during their period.
Studies have also found that IBS occurs 2 to 6 times more often in women than men, however, the underlying reason for which women have an increased vulnerability to IBS remains largely unknown.
IBS may stem from various other factors. One such factor of IBS is when the immune system in the gut doesn't work correctly. The immune system's job is to protect the body, but in IBS, it might react too much to certain things, causing inflammation and irritation in the digestive system.
Moreover, an imbalance in gut bacteria can contribute to the symptoms of IBS. It's important to note that while bacteria are essential for the proper functioning of the gut, an overabundance of certain types of bacteria can lead to disruptions that trigger IBS symptoms.
Another factor involves irregularities in gut movements, which can disrupt the absorption of nutrients. In individuals with IBS, the gut can move too much or too little, leading to changes in bowel movements. However, it's important not to diagnose yourself because there are other conditions that can look like IBS. For example, problems like celiac disease, giardia, or even colon cancer need to be ruled out by a doctor before concluding its IBS. So, seeking professional help is crucial for accurate diagnosis.
3. Constipation
What is constipation?
It is often believed that constipation refers solely to decreased frequency of bowel movements, but it can also just be difficulty passing stools or hardened stools.
Constipation is also the most common digestive complaint in the United States. A study of 15,014 individuals found that constipation was frequent in 18.2% of women.
What causes constipation?
Constipation has common causes, let’s take a look at some:
- Lack of Exercise: Sedentary lifestyles and a lack of regular physical activity can significantly impact bowel movements. Physical movement helps stimulate the muscles of the intestines, promoting healthy contractions that propel stool through the digestive tract. Without adequate activity, these contractions can slow down, leading to constipation.
- Medications: Some medications can disrupt the normal patterns of the digestive system, leading to constipation as a side effect. Certain pain medications, antidepressants, antacids with calcium or aluminum, and iron supplements are known to potentially cause constipation by affecting muscle contractions or water absorption in the intestines.
- Insufficient Fiber in the Diet: Fiber is essential for maintaining proper bowel function. It adds bulk to stool and helps maintain regular bowel movements. Diets low in fiber can result in harder and drier stools, which can be difficult to pass. Whole grains, fruits, vegetables, and legumes are good sources of dietary fiber that aid in preventing constipation.
- Not Drinking Enough Water: Staying hydrated is crucial for softening stool and facilitating its movement through the intestines. Inadequate fluid intake can lead to stools that are harder and more challenging to pass. Drinking enough water helps maintain the right consistency of stool, making it easier for the body to eliminate waste.
- IBS: IBS is a chronic disorder that can cause various digestive symptoms, including constipation. The complex interactions between the gut and the nervous system in individuals with IBS can lead to irregular bowel patterns, including constipation.
- Ignoring the Urge to Use the Restroom: Ignoring the body's natural signals to have a bowel movement can lead to constipation. Over time, delaying or suppressing the urge to use the restroom can cause stool to become harder and more difficult to pass. It's important to listen to your body's signals and respond to them promptly.

You may also experience constipation during your menstruation due to the rise in progesterone levels. Progesterone, a hormone essential to your reproductive system, slows down your digestive system, making it harder to have regular bowel movements.
4. Gallstones
What are gallstones?
Gallstones are hard and small crystalline masses formed in the gallbladder from cholesterol, bile pigments, or calcium salts. When these pebble-like pieces block your bile ducts, sudden and intense pain can occur.
This can often happen after eating a fatty meal, as the gallbladder contracts to release bile to help digest fats. As a result, the pain can come on suddenly and might be felt in the upper right side or middle of the abdomen. The discomfort can also radiate to the back or right shoulder.
While gallstones do not always require immediate treatment, they can lead to severe discomfort and complications if left untreated. If attacks of pain are frequent, or if the pain does not resolve on its own, seeking medical treatment is crucial.
Although not everyone with gallstones experiences symptoms, abdominal pain or nausea can signal their presence. The key factor is the presence of severe or unrelenting pain. Pain coupled with fever, or yellowing of the eyes or skin can indicate a medical emergency, requiring prompt medical care.

What causes gallstones?
The exact cause of gallstone formation is not always clear. Still, it is generally attributed to an imbalance in the composition of bile, a digestive fluid produced by the liver and stored in the gallbladder.
Sex hormones are most likely responsible for the increased risk of gallstones in women. Estrogen increases cholesterol levels in bile, making fluid more sludge-like and more difficult for the gallbladder to empty completely. The effect is much greater in pregnant women, as well as those taking birth control pills or hormone replacement therapy.
In the United States, gallstones occur in up to 20% of women by the age of 60. Additionally, women tend to have higher levels of body fat in comparison to men. This increased body fat can lead to more cholesterol entering the bile, promoting gallstone development.
5. Inflammatory Bowel Disease (IBD)
What is IBD?
IBD includes Crohn's Disease (a chronic disease that causes inflammation in the digestive tract) and Ulcerative colitis (a chronic disease that causes inflammation in ulcers in the inner lining of your large intestines).
A CDC study of 3.1 million U.S. adults showed that the prevalence of IBD was higher among women (1.5%) than men (1.0%). Symptoms of IBD include diarrhea, blood in stool, anemia, and weight loss.

What causes IBD?
In understanding the factors that contribute to the development of IBD, it's important to note that the exact mechanisms and interactions between these factors are subjects of ongoing research. Furthermore, IBD is a complex condition that varies greatly among individuals in terms of its presentation and severity.
Hormonal influences–like estrogen–can impact immune responses in women, who generally have more active immune systems. This may contribute to the development of autoimmune diseases like IBD.
Genetic predispositions also play a key role in IBD development. Certain genetic variations have been associated with the increased risk of IBD, with some genes being found on the X chromosome. These variants may affect response to treatment, disease behavior, and the risk of complications associated with IBD.
How can you manage and maintain a healthy gut?

Maintaining healthy habits keeps your digestive system happy and healthy. There are some key things you can do to maintain a healthy diet in order to keep your digestive system functioning properly: drink adequate amounts of water, eliminate as much processed food as possible, eat foods high in fiber, and exercise regularly (even just walking counts!).
Women often manage significant stress in their personal and professional lives. Stress can increase inflammation in the gut and even alter the balance of gut bacteria. This is why learning to handle stress healthily is essential to improving your GI issues. Some stress management techniques include physical and relaxation exercises, seeking support, and self-care activities.
Conclusion
By understanding the complexity of women's digestive health, we can paint a more comprehensive picture of women's GI challenges.
Remember, you are not alone in experiencing any of these challenges, and just because you are a woman does not necessarily mean you will get any of them. However, it is important to stay informed of their symptoms in order to seek support from healthcare professionals if needed.
Empower yourself with knowledge, listen to your body, and track your symptoms to gain valuable insights and guidance on managing these conditions.
By nurturing your gut, you are nurturing your overall health and well-being as a woman.