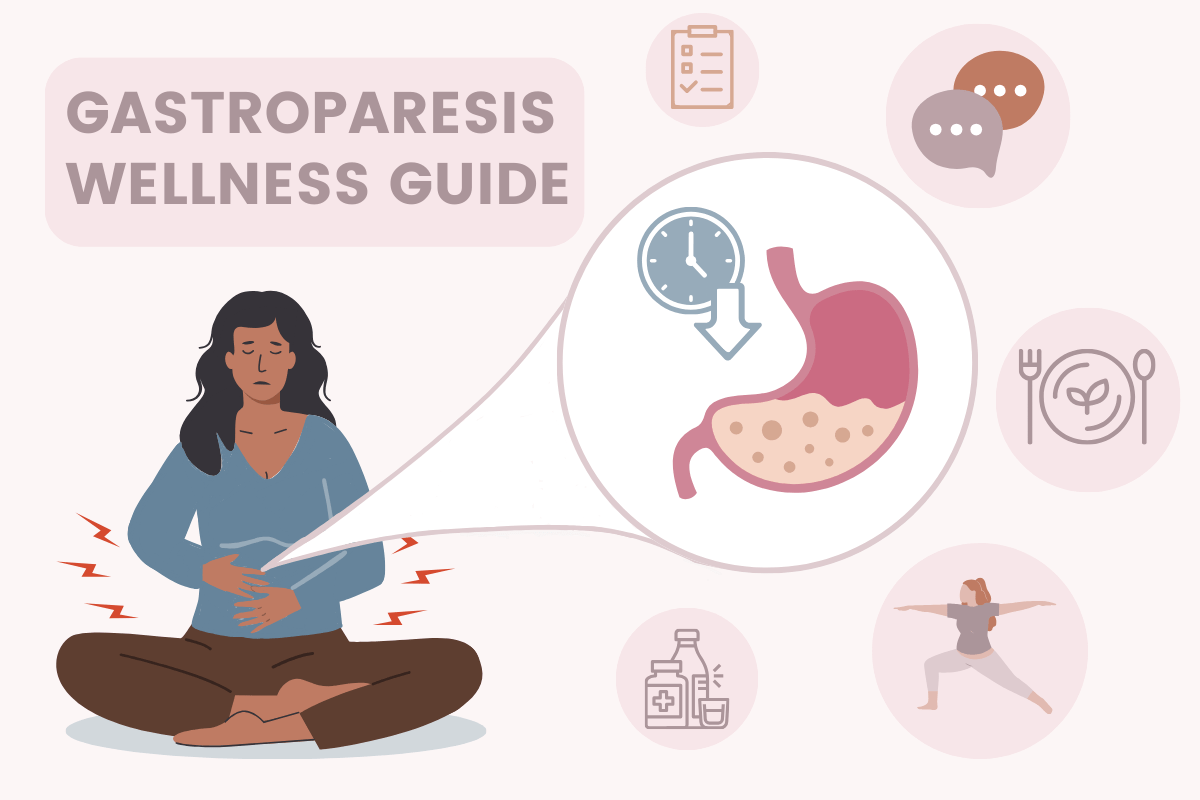
Living with gastroparesis can be overwhelming, but thankfully, with the advent of online resources and patient communities, you don't have to face it alone. In this article, we’ll explore the key organizations, educational platforms, support communities, and evidence-based coping strategies to help you navigate gastroparesis.
Gastroparesis is the term used to describe the paralysis of your stomach muscles, which, as you can imagine, significantly impacts daily life. Patients with gastroparesis are likely familiar with symptoms like nausea, vomiting, bloating, and abdominal pain. For those with severe cases, gastroparesis tends to take a hefty physical and emotional toll. In light of that, our aim is to connect patients with the proper resources and support to manage this condition.
What is Gastroparesis?
To understand what gastroparesis is, it's important to understand how digestion usually works. Normally, muscles called 'smooth muscles' contract to move the food you eat along your digestive tract. Anytime you contract a muscle, whether that be consciously or unconsciously, your nervous system is involved. Your nervous system is the brain-to-muscle connection that's responsible for everything from walking around to digesting your food.
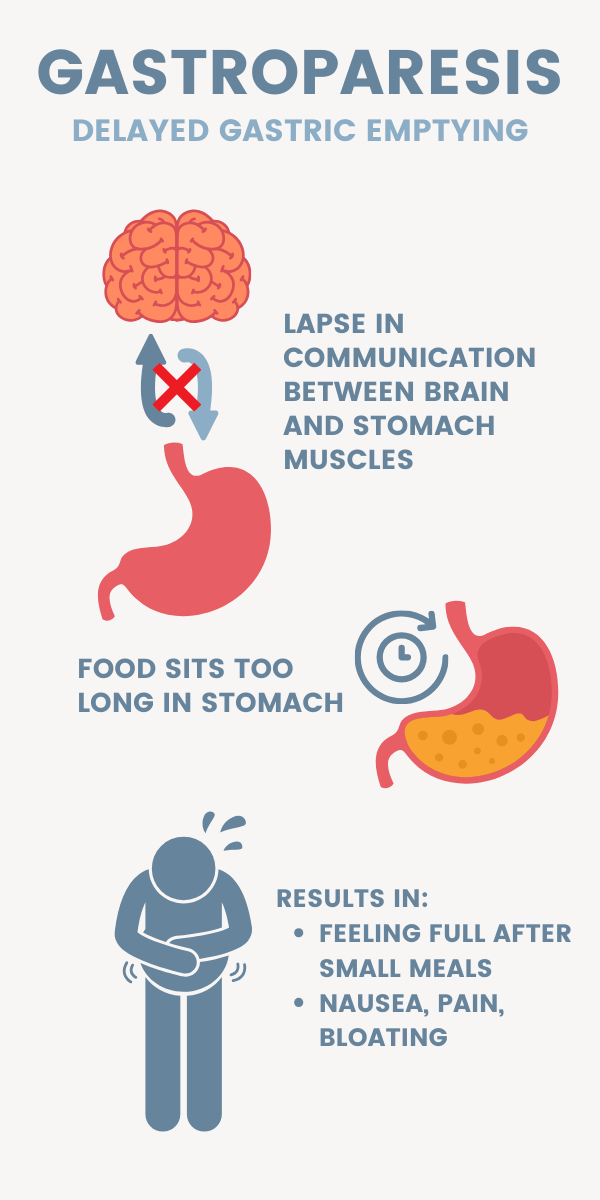
For patients with gastroparesis, there's usually a lapse in communication between the smooth muscles in your digestive tract and the nervous system that controls it. As a result, food sits in the stomach for much longer than normal, and in turn, patients feel full for longer. This delayed removal of contents from the stomach, or “gastric emptying,” is what can lead to nausea, pain, and bloating.
The “gut paralysis” that occurs in gastroparesis can be caused by a variety of factors that affect the stomach or nervous system. Some of these include diabetes, past gastrointestinal surgeries, medications, neurological conditions, or other conditions like Ehlers-Danlos Syndrome.
Symptoms of Gastroparesis
Like many gastrointestinal (or GI) disorders, gastroparesis is no simple illness. It can cause nutritional deficiencies, weight loss, and not to mention a decrease in quality of life. These symptoms can vary from person to person, and like many chronic illnesses, some may experience mild ones, while others have severe daily symptoms.
The most common symptoms of gastroparesis are nausea, vomiting, bloating, and feeling full after small meals. Some might also experience heartburn, abdominal pain, or a loss of appetite.

Which Doctors Treat Gastroparesis?
Proper diagnosis of gastroparesis requires a thorough evaluation by a doctor who specializes in the digestive tract, otherwise known as a gastroenterologist. Many patients also work with dietitians or nutritionists to create dietary plans that are tailored to their specific needs.
How is Gastroparesis Diagnosed?
Your evaluation may include a physical exam, blood tests, imaging studies, and gastric emptying studies. Due to the many factors involved in proper digestive function, it’s often difficult for providers to pinpoint a cause, in which case, you might hear it referred to as idiopathic gastroparesis.
To test if your stomach isn’t digesting food fast enough, your doctor may perform what’s called a gastric emptying study. This involves keeping track of a tiny amount of radioactivity that you ingest before the test. Imaging tests can also show any blockages that could be preventing proper digestion, therefore ruling out gastroparesis as a cause for discomfort.
Your doctor will probably ask you about your medical history and current medications as well. This is because some medications that are intended to treat other conditions can have side effects that result in gastroparesis. Recent studies suggest that certain weight loss drugs like Wegovy and Ozempic are tied to gastroparesis. These drugs both contain semaglutide as an active ingredient, which helps with weight loss by slowing down digestion. In severe cases, they can slow digestion too much and cause unintended gastrointestinal problems, including gastroparesis.
Diet and Nutrition: Tips for finding gastroparesis-safe foods
Because gastroparesis interferes with digestion, it’s important that you’re eating and drinking things that your stomach can easily digest. The National Institute of Diabetes and Digestive and Kidney Diseases reports that symptoms can be subdued by aiming for small, frequent meals throughout the day, rather than three large meals. Even for those without gastrointestinal issues, foods high in fat and fiber are harder to digest. So, to avoid gastroparesis flare-ups, clinical data suggests that it’s also best to avoid these meals.

Here’s a summary of some more helpful tips for creating gastroparesis-friendly meal plans from the International Foundation for Gastrointestinal Disorders:
- Eating slowly and chewing food thoroughly
- Drinking plenty of fluids throughout the day
- Avoiding carbonated beverages and alcohol
- Choosing foods that are soft and easy to digest, such as cooked vegetables, lean protein, and low-fat dairy products
Working with a registered dietitian who specializes in gastroparesis can be helpful as well, especially in the case of diabetic gastroparesis, wherein both conditions need to be managed carefully. Here are some helpful resources for nutrition and diabetic gastroparesis:
- Univ. of Virginia: Diet Intervention for Gastroparesis and Diabetes Mellitus
- Diabetes Care Community: Gastroparesis Diet and Diabetes
Gastroparesis Treatment: Exploring medical and lifestyle interventions
In the case that nutritional changes don’t get rid of your symptoms, there are some alternative options for the treatment of gastroparesis, those of which depend on symptom severity and underlying cause. In some cases, your doctor might recommend medication or surgical interventions that stimulate stomach movement since your stomach can’t contract on its own.

Medications for gastroparesis
Medications that can be used to treat gastroparesis in severe cases include prokinetic agents, which help stimulate the stomach muscles to contract and move food through the digestive tract. Antiemetic medications can also be used to control nausea and vomiting.
Gastroparesis surgery
In severe cases, surgical interventions like gastric electrical stimulation may be used. This involves the implantation of a device that delivers electrical impulses to the stomach muscles, which can help stimulate stomach motility (or smooth muscle contraction) and move food along artificially.
Gastroparesis Support Groups and Online Communities
Connecting with others who understand your day-to-day struggles can be incredibly beneficial for your mental health when dealing with gastroparesis. There are numerous online support groups and communities just for patients and their caregivers.

These groups provide a safe space for individuals to connect, share experiences, and offer support and guidance. Some popular support groups for gastroparesis include the Gastroparesis Support Group on Facebook and the Gastroparesis Patient Association for Cures and Treatments.
By building relationships with those who share your experience, there’s an opportunity to learn about other unique journeys and different coping strategies. A dialogue around potential treatment options and nutritional habits is also important for staying active in your health management.
Educational Resources for Gastroparesis
The Internet provides a wealth of informational resources for individuals with gastroparesis and their caregivers. These resources provide in-depth information on the condition and its management, as well as tips for coping with symptoms.
Some popular educational resources for gastroparesis include:
- The International Foundation for Gastrointestinal Disorders
- The National Institute of Diabetes and Digestive and Kidney Diseases
- The G-Pact organization blog
Coping Strategies and Self-Care for Gastroparesis
Dealing with gastroparesis day in and day out can be both mentally and emotionally draining. Luckily, there are a variety of coping strategies that you can try out to see what works best for you.
Here are a few coping strategies specific to gastroparesis:

Exercise and yoga for gastroparesis. Depending on the severity of your condition, there are certain exercises and movements you can take to help stimulate muscle contraction. Here’s a Youtube video that’s well-reviewed by gastroparesis patients. It should be a good place to start if you’re interested in using yoga to alleviate symptoms.
Mindfulness, meditation, and relaxation techniques. Stress and anxiety are often to blame for flare-ups of all kinds of illnesses, and gastroparesis is no exception. This review of psychology and associated gastroparesis found that stress and anxiety are positively correlated with gastroparesis symptoms. The authors also found that psychological intervention can improve gastric function and depression, although these studies are somewhat limited. During times of high stress or anxiety, doing guided meditations and taking actions to de-stress may help to relax the nervous system and keep symptoms manageable.
Seeking support from friends and family, as well as professional counselors are powerful tools for managing your gastroparesis. Being transparent about your condition can help those around you to better understand your needs and strengthen your coping strategies.
Logging symptoms and flare-ups. By keeping track of what foods or activities worsen symptoms, it will become easier to know what triggers your gastroparesis pain. You can do this by keeping a journal, or by using food or symptom-tracking apps.
Guava allows you to track things like symptoms, food and drink intake, bowel movements, and more. It also syncs with your health-monitoring devices to track other data like activity and blood glucose. It automatically tells you about statistically significant correlations so that you can better understand your condition. Here’s a more thorough explanation of how you can use guava to discover more about your symptoms.


Empowering Individuals with Gastroparesis.
Although it's challenging, the proper resources and support can get you on track to managing gastroparesis. It's important to work closely with healthcare providers to make a comprehensive treatment plan that’s tailored to your needs. Keep in mind that by prioritizing self-care and coping strategies, it'll become easier to manage the emotional toll of gastroparesis.
We hope that by getting involved in advocacy and awareness efforts, we can help advance our understanding of the condition and improve treatment options and support for gastroparesis patients, both now and in the future.