This is article five in a seven-part series addressing gender bias in the healthcare system.
As many have said before, we must reflect upon our past when trying to improve the future. Our history often exposes much about the current issues we are struggling with and can even reveal how to solve them. Therefore, to truly understand the topic at hand, we must first imagine our healthcare system several decades prior.
As strange as it seems, the 1990s brought more than just ‘Friends’ and grunge to the US. They also brought a huge push for women’s rights in healthcare. Several years before, women began to voice concerns over inequality in clinical trials. As a result, in 1986, the National Institutes of Health established a policy that required all studies to include women or have a reasonable explanation as to why they weren’t included. Finally, as the ’90s approached, political pressure was placed on the medical field to learn more about women’s health.

Before this large push, there were few resources and funding for women’s health research. As a result, women were dying from well-known diseases that doctors would simply miss. Cardiology was one field in particular where this was quite prevalent.
While writing these articles, I had the opportunity to talk to Dr. Carl Jr. Szot, MD, a cardiologist who was right in the thick of it all. According to Dr. Szot, scientists and doctors failed to realize that women with heart disease displayed different symptoms than men. The commonly known symptom of heart disease is chest pain, but there are several other less well-known symptoms, such as jaw pain, nausea, arm pain, and shortness of breath. Unfortunately, women with heart disease tended to show up with these less well-known symptoms, causing doctors to misdiagnose the disease.
Dr. Szot remembers from the ’90s. “Half of the women coming in for second opinions had heart disease and had just been blown off.”
Women were testing positive for heart disease and still being told it wasn’t the issue, that it was all in their heads. Instead, doctors would blame these symptoms on stress or anxiety, a problem you may recognize from my earlier articles.
Now, the field, in Dr. Szot’s opinion, has gotten much better. Women are included in far more research than they used to be (though the numbers are still not equal), and misdiagnosis is not as common. When asked what he attributes to this success, he agreed more female clinical trials helped, but equally important was more female cardiologists entering the field.
“I was trained by female cardiologists, which was rare back then.” Dr. Szot pointed out, which helped him better advocate for women’s heart health. In Dr. Szot’s opinion, more female cardiologists changed the field’s complexion and added a new perspective.

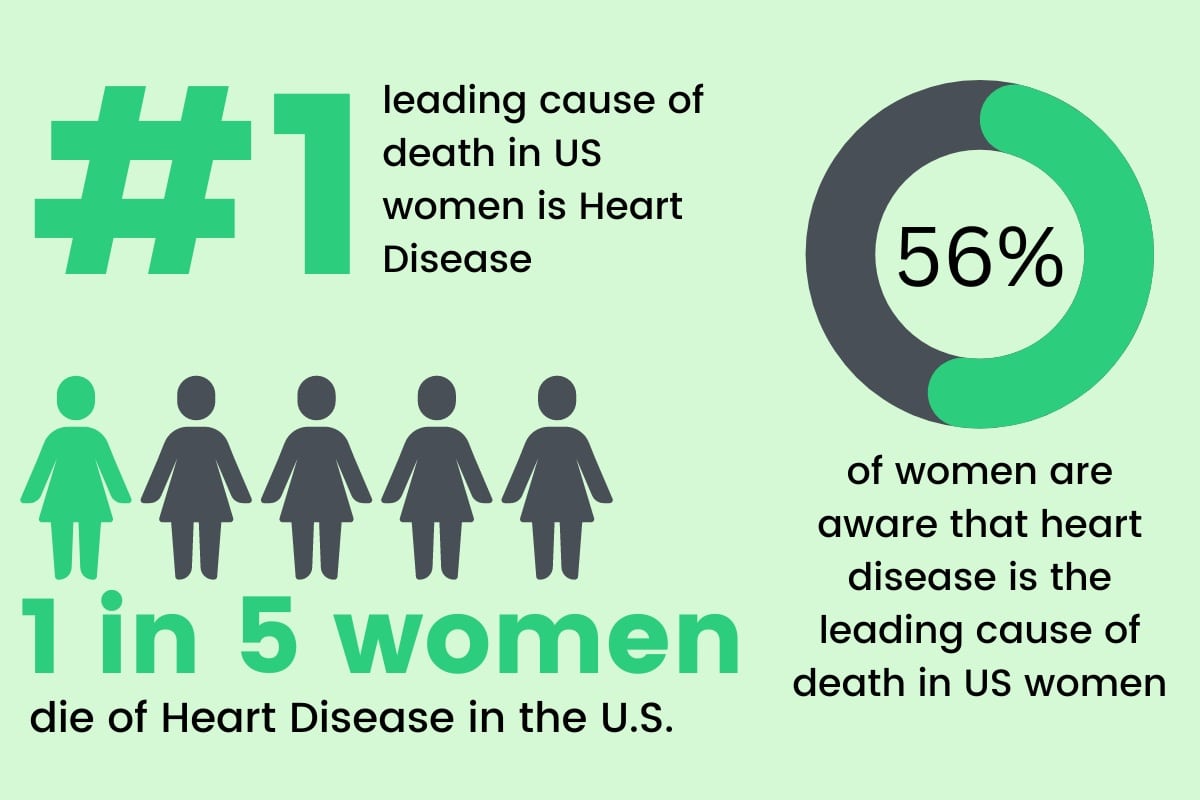
However, as much as this issue has improved since the 90s, it still exists today. Women aren’t represented equally in clinical trials and are still underdiagnosed for conditions like strokes and heart attacks. Heart attacks, specifically, are still understudied and often portrayed as a male disease. This stigma diverges both female patients and doctors from the diagnosis of heart disease. Yet, according to the CDC, heart disease is the “leading cause of death for women in the United States.”
Often bias can cloud people’s judgment, even in the medical field. To avoid this, Dr. Szot offered some closing advice. Don’t be afraid to ask questions. Sometimes doctors can find themselves on one train of thought without considering another. Tell them your concerns, thoughts, or inklings. Even if you aren’t right, there’s always the possibility that you could be.
Awareness of this topic is vital. Even after several decades of increased efforts to include women in research, we must understand that there’s still more ground to cover. For instance, as Dr. Szot pointed out, women still tend to do worse than men after a heart disease diagnosis. There are many speculations surrounding these statistics. For example, atherosclerosis (the build-up of plaque along artery walls that can cause heart attacks, strokes, etc.) is different in women than in men. Women have smaller blood vessels, higher bleed rates, and are often older when the disease shows up.
There’s more research happening now on this topic than there ever was, but we must remember we are still behind. Men have been at the pinnacle of research since the beginning of time, while women have been playing catchup since the start of the 1990s. Therefore, as a female patient advocating for yourself, it’s important to remember that the centuries of human health research prior to this movement barely include us.